Researchers report that cognitive impairment caused by severe COVID-19 is comparable to an average 20 years of aging, equivalent to an IQ drop of 10 points. Study results reveal its effects can still be detected up to six months post acute illness; recovery will occur gradually over time.
Evidence indicates that COVID-19 can lead to long-term mental and cognitive health problems in recovered individuals, with symptoms including anxiety, sleep disturbances, fatigue, word recalling problems and post-traumatic stress disorder appearing months post infection. A recent survey indicated that 1 out of 7 individuals experienced cognitive issues 12 weeks post positive COVID-19 tests.
Even minor cases can result in chronic cognitive symptoms; between 33% and 74% of hospitalized individuals report experiencing these issues three to six months post hospitalization.
To explore this relationship more comprehensively, data were analyzed from 46 patients who received hospital care for COVID-19 in either an intensive care unit or on a ward, of whom 16 received mechanical ventilation while in hospital.
Patients were provided comprehensive cognitive tests approximately 6 months following acute illness using the Cognitron platform to measure reasoning, attention and memory capabilities as well as scales that measured PTSD depression and anxiety.
COVID-19 survivors exhibited less accuracy and slower response times when compared to their matched control individuals, and these deficits could still be detected six months later when individuals were monitored again. Individuals needing mechanical ventilation were most significantly impacted. When compared against the general population (66,008 individuals in all), cognitive loss magnitude equivalent to 20 years of aging has been estimated as being equivalent to an IQ loss of 10 points.
Surviving COVID-19 caused survivors to score poorly on tasks requiring verbal analogical reasoning, supporting what has often been reported: difficulty finding words. Processing speeds also decreased significantly – in line with prior post-COVID-19 observations of decreased glucose consumption by their frontoparietal network (which oversees working memory, complex problem solving and attention, amongst other functions).
Researchers concluded that cognitive impairment is common across a range of neurological conditions and normal aging processes; however, in this particular study cognitive patterns appeared which were different than any other disorders studied.
Though it is well-established that individuals recovering from severe COVID-19 can present with numerous poor mental health symptoms, including disturbed sleep, low mood, lack of motivation and post-traumatic stress, anxiety depression and fatigue, the researchers found that cognitive deficits were best predicted by severity of acute illness.
Scores and reaction times began improving slowly over time for patients; however, any cognitive faculty recovery was gradual at best and was probably affected by various factors including illness severity as well as its psychological or neurological ramifications.
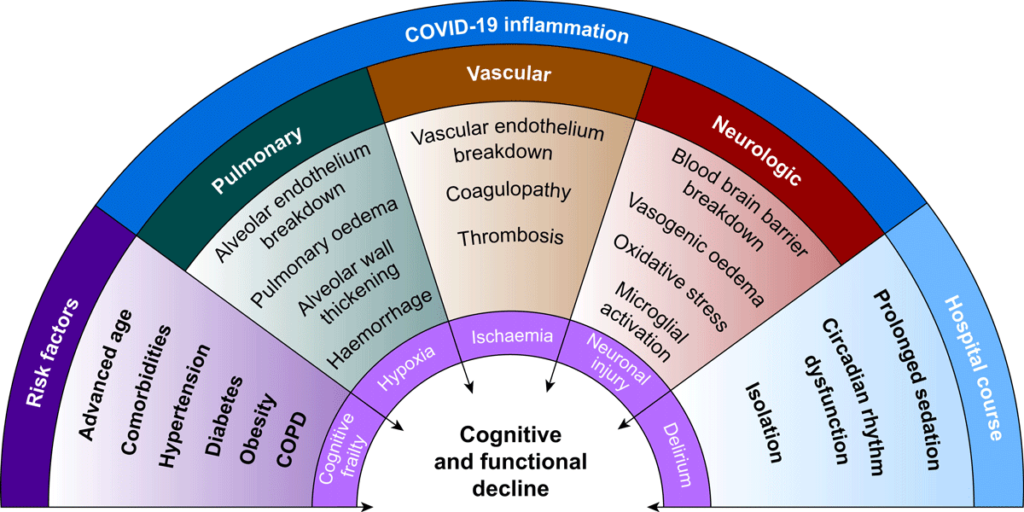
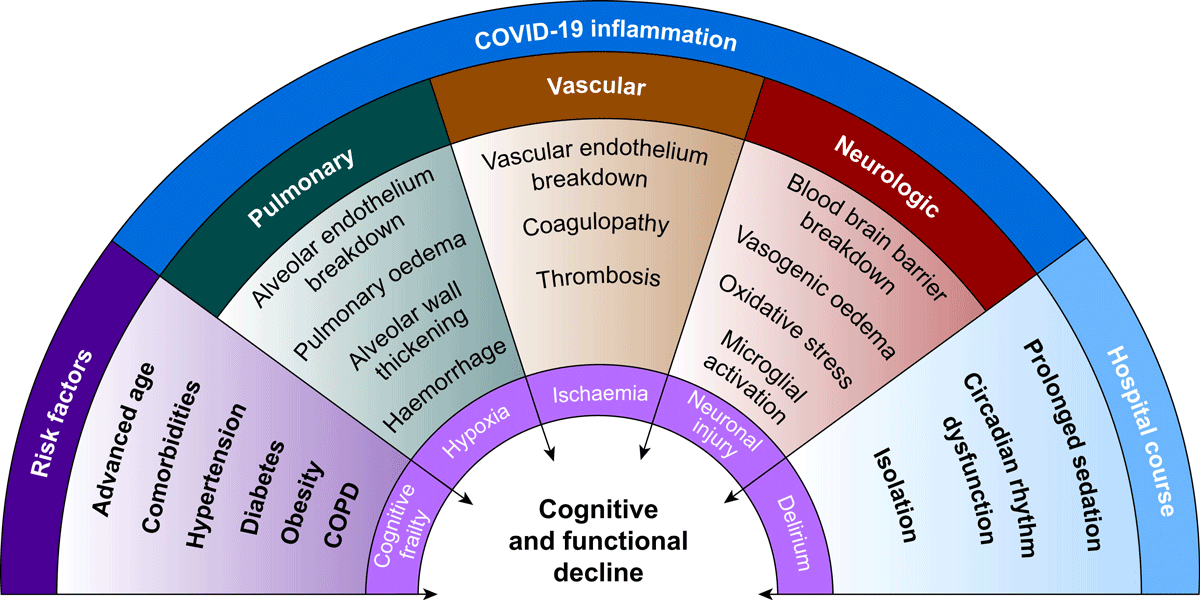
Researchers state that numerous factors could contribute to cognitive deficits. Direct viral infection could play a part, though unlikely as a main culprit; rather it’s likely a combination of contributing factors such as blocked small or large blood vessels due to clotting, insufficient oxygen supply to the brain, or microscopic bleeds may all play their part. Emerging evidence points towards damage due to inflammation caused by both immune system response and body processes as being key drivers of cognitive decline.
Even though this study focused solely on hospitalized COVID-19 cases, researchers note that those without severe symptoms could also show mild impairment.